The Vital Role of U.S. Foreign Aid in Global Health
Wagner Foundation Founder and President Charlotte Wagner shares her thoughts on how foreign aid transcends the notion of charity, and the ripple effects of a freeze in funding.
Every one of us should have the opportunity to attain and live a truly healthy life.
We believe health is a fundamental human right. But we know that barriers to good health are complex, and that healthcare delivery is just one part of the equation. Health outcomes are highly tied to the environments where people live, learn, work, and play. The same social, economic, and political privileges and disadvantages that drive inequality also have an outsized impact on our health.
At Wagner Foundation, we strive to expand equitable access to health by collaborating with health institutions and leaders both in the US and around the world addressing the gaps in care delivery, financing models, as well as the social drivers of health.
We’re proud to partner with organizations operating at the intersection of clinical health and public health systems, as well as those that are tackling the underlying systemic factors that impact wellbeing and health equity.

Wagner Foundation believes health is a human right. Yet, individuals living at the last mile of rural, impoverished communities do not often have access to that right and most need to travel over 5 km to reach the nearest health facility. Healthcare systems and financing models in these geographies are underdeveloped and broken, perpetuating the poor health conditions of these communities, majority of whom are farmers.
We believe that all governments should have the funding they need to shape their national health priorities and improve the wellbeing of their citizens. However, many low- and middle-income countries (LMICs) face high debt burdens which limit their ability to invest in their health systems. In fact, nearly half of the world’s population lives in countries that spend more money servicing their debt than they do investing in healthcare. Additionally, well intentioned external aid coming into countries is often fragmented and may not align with the government’s national priorities. This has significant implications on countries’ ability to enhance their health systems and allow their people to access good health — especially in the face of compounding crises like climate change and conflict.
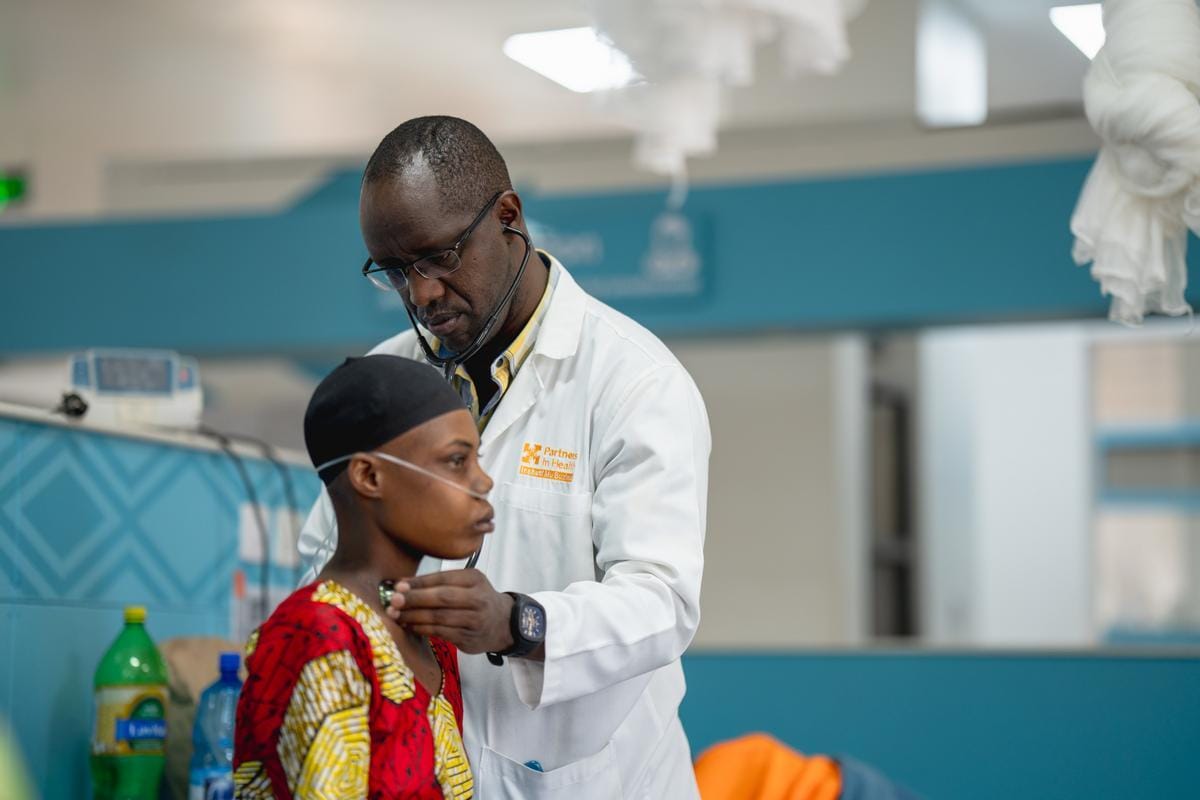
We focus our efforts in Africa, Latin America, and Haiti, striving to build fully resourced and integrated public health systems aligned with national priorities. Our funding is also particularly focused on building a professionalized, local health workforce at all levels of care as we know that health systems are made up of people, and they need to be resourced and supported to deliver high-quality care.
We recognize the importance of adequate health financing to transform health systems in LMICs. By partnering with organizations advocating for increased and innovative health financing models to support national health priorities, we believe we can help create an environment that allows governments and international institutions to deliver on the promise of healthcare access to all.
We are committed to achieving good health and wellbeing for all. Yet, over half of the world’s population lacks access to the full range of quality health services needed to lead a dignified life. Many families live in hard-to-reach remote areas or cannot afford the high out-of-pocket costs of healthcare. And even in geographies where health services are readily available, the limited capacity of the health workforce and poor infrastructure can affect the quality of care.
As a result, people living in poverty in rural and remote communities around the world are at a disproportionately higher risk of poor health outcomes. At the root of this disparity is broken health systems and stalled progress towards universal health coverage.
That’s why we partner with organizations that are strengthening health systems at all levels by training the health workforce, developing health infrastructure like adequately equipped facilities where care is delivered and efficient data management systems informing decisions, and advancing evidence-based policies to improve public health. The organizations we support work in lockstep with national Ministries of Health to ensure they are advancing the health priorities of the countries where they work while also providing technical assistance and capacity support to the government to see those priorities through.
By building stronger health systems, we can help create a world where everyone has access to quality healthcare, regardless of geography or ability to pay.
Health systems are made up of people and they need to be adequately resourced and supported to deliver high-quality care. However, health workers at all levels of care (community, primary, tertiary) are underfunded and therefore lack the necessary tools and resources to deliver quality medical care to their patients. This is particularly true in rural communities where we work. Community Health Workers (CHWs), 70% of whom are women and are essential in making sure remote communities receive the care they need, have been historically under supported, often expected to volunteer their time for little to no pay. Approximately 50% of CHWs in low-to-middle-income communities are unsalaried.
In addition to the inadequate support provided to the health workforce, there is also a major gap in the number of health workers, with the WHO estimating a global shortfall of ten million health workers by 2030.
At Wagner, we support organizations centering the health workforce, both clinical and non-clinical, as an essential driver of advancing health equity. This includes nurses and midwives delivering critical maternal and infant care, community health workers serving the hardest to reach families, and biomedical engineers ensuring medical equipment is functioning and maintained over time. Our funding focuses on advancements in access to and quality of training across the public health system as well as organizations advocating for national policy that calls for the professionalization of the health workforce.
We believe that a fully resourced and supported global health workforce is vital in ensuring health as a human right for all.

The US spends more on health care than any other nation—yet has the worst life expectancy among its high-income peers. It’s also the only developed country that doesn’t guarantee health care to its people. Nowhere is this failure more glaring than in maternal health—American mothers die at more than twice the rate of those in other high-income nations. Put in perspective, if pregnancy and birth were a job, it would be one of the ten deadliest occupations in the country.
So why does the US spend more on health care than any other nation, yet get so little in return? 80% of health outcomes are shaped by non-medical factors—like housing, education, healthy food, and stable employment—yet the US funnels spending into medical care that influences just 20% of health outcomes. The research is clear, health starts beyond the clinic—but in a system without universal coverage, profit drives treatment, rather than prevention.
We require new models that meet the needs of diverse communities who have been overlooked and failed by our current health system. This calls for the development of a human-centered process that integrates the voices of those most affected by inequitable health institutions into the transformation of care both within and beyond the clinic.
No woman should die from childbirth. Yet in the US—a nation that spends more on healthcare than any other—the maternal mortality rate is more than double, sometimes triple, that of other high-income countries. The disparities are even starker for Black women, who are more than three times more likely to die from pregnancy-related complications as white women, according to the CDC in 2023. And despite all of this spending, one-third of U.S. counties are obstetric deserts—lacking a single birthing facility or obstetric provider. These gaps don’t just impact where a woman gives birth but also limit access to critical prenatal and postpartum care.
This crisis isn’t inevitable, but we do need to reimagine maternity care in the US, expanding access to safe, patient-centered, community-based models. This is why at Wagner Foundation we are investing in birth centers, midwives, and doulas as essential components of this shift. The evidence is clear: investing in community birth infrastructure improves outcomes, enhances patient satisfaction, and lowers costs.
By expanding midwifery access and investing in birth equity, we can ensure that every person giving birth receives the compassionate, high-quality care they deserve—regardless of race, income, or zip code.
Your zip code should not be a better predictor of your health than your genetic code. But when it comes to health, place matters. 80% of health outcomes are shaped by the environments where people live, learn, work, and play often referred to as the social drivers of health (SDOH). These social drivers of health—including housing, education, access to healthy food, and stable employment—matter far more than medical care, which influences only 20% of health outcomes. Evident here in Boston—home to some of the nation’s best health institutions—where there is a 23-year gap in life expectancy between Roxbury and Back Bay, two neighborhoods just a few miles apart.
At Wagner Foundation, we are investing locally to bridge the gap between hospitals and communities, ensuring that health care extends beyond the clinic walls. We support the development of new care delivery models that connect patients directly to essential services—food prescriptions, housing assistance, and other resources that address unmet health-related social needs. At the same time, we work with hospitals and health systems to close resource gaps at the neighborhood level. This means fostering collaboration and driving direct investment in community infrastructure—from affordable housing and healthy food access to good jobs and wealth-building opportunities.
By embedding health care systems within the fabric of communities, we are working towards a future where health is not dictated by zip code but sustained through collaboration and sustained investments in people and place.
We center artists as catalysts of change and community development through local and national investments in contemporary visual art exhibitions, publications, public art, and visual arts organizations at all scales.
We collaborate with partners to expand access to wealth-building opportunities and create pathways to fair wages, ensuring everyone has the resources they need to thrive.